
What is Keratoconus and how does it differ from other eye conditions?
Keratoconus is a progressive eye disease that affects the cornea, causing it to thin and gradually bulge into a cone-like shape. Unlike common eye conditions like nearsightedness or astigmatism, which can be corrected with glasses or contact lenses, advanced keratoconus distorts vision so severely that standard lenses may not provide clear vision. Over time, the irregular shape of the cornea leads to blurry, distorted vision, and in extreme cases, may result in scarring that requires surgical intervention.

Dr. Angie Wen, Doctor of Ophthalmology
How can eye rubbing contribute to Keratoconus?
Eye rubbing is a common but harmful habit, especially for those prone to keratoconus. Patients with this condition have weak collagen fibers in the cornea, making it more susceptible to shape changes from external pressure. Excessive eye rubbing can accelerate the progression of keratoconus by further weakening the corneal tissue. It’s essential to manage allergies or other conditions that may lead to frequent rubbing, as this can significantly worsen the condition over time.
Why are individuals between 14 and 35 more vulnerable to Keratoconus?
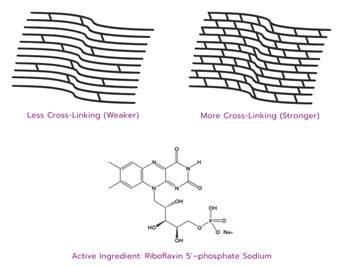
Keratoconus typically begins in teenagers and young adults, progressing rapidly through the 20s and 30s. During this period, the cornea is more flexible and susceptible to changes. Natural collagen cross-linking, which occurs with age and UV light exposure, strengthens the cornea, often halting progression in the mid-40s. Early diagnosis is critical for young individuals, as treatments like corneal cross-linking (CXL) can stop the disease from advancing if caught early.
What are the early signs of Keratoconus?
Signs of keratoconus include a rapid increase in prescription strength or difficulty achieving clear vision despite updated glasses or contact lenses. If your vision becomes progressively worse over a short period or cannot be corrected with standard lenses, it may be time to consult a cornea specialist. Early detection through specialized corneal imaging can significantly improve outcomes and prevent long-term damage.
What advancements in treatment are available for Keratoconus?
In the past, patients with keratoconus had limited options, often relying on rigid gas permeable lenses to improve vision. However, recent advancements, such as FDA-approved corneal cross-linking (CXL), have revolutionized treatment by slowing or halting the progression of keratoconus. Other procedures, like Cornea Tissue Addition Keratoplasty (CTAK), can reshape advanced cases, and Laser Vision Correction (LASIK) is being studied as an option post-CXL. Early diagnosis and treatment can preserve vision and reduce the need for future surgery.
More information on Dr. Angie Wen:
Dr. Angie Wen is a highly regarded Associate Professor of Ophthalmology and a Cornea and Refractive Surgeon at the prestigious New York Eye and Ear Infirmary of Mount Sinai in New York City. With extensive expertise in treating complex corneal conditions, Dr. Wen specializes in performing corneal transplants, refractive surgeries like LASIK, and advanced cataract surgery. Her exceptional skills and dedication to her field have earned her a leadership role as the Cornea Fellowship program director, where she plays a key part in shaping the future of ophthalmology. In addition to her surgical work, she is deeply committed to teaching and mentoring the next generation of eye surgeons, guiding residents, fellows, and medical students through their clinical and surgical training. Dr. Wen’s contributions to ophthalmology are not only in her clinical practice but also in her dedication to research and education, making her a respected figure in the field.



More Stories
Besties to Bae? Brenda & Derek’s Endgame Dilemma
👓 A Clearer View: How We Dealt With Poor Vision Before Eyeglasses
Beyond the Bouquet: Thoughtful Mother’s Day Gift Ideas She’ll Truly Cherish